Between work, city traffic, and food habits, do you ever just feel… off? And more likely you may not always pin it to specific sickness. Sometimes it’s a nagging sense of fatigue, other times it’s a general achiness in your joints, a bit of brain fog that makes it hard to focus, or a feeling of being puffy and bloated.
If this sounds familiar, you’re not just “getting older” or “too stressed”. It’s a little more complicated than that. You are likely feeling the whispers of a single, powerful biological process that has become a central concern of modern health: inflammation.
Before we go any further, let’s be very clear about one thing: inflammation is a biological marvel. It isn’t inherently bad. Inflammation is one of your body’s most essential tools for survival. The confusion and the danger lie in its two very different forms.
What is inflammation?
Inflammation is a process- your body’s process of diligently monitoring and protecting itself from any internal or external harm, 24 by 7. Yes, internal too. On a microscopic level, a human body is constantly dealing with minor wear and tear. Old cells die and need to be cleared away. Tiny metabolic byproducts need to be disposed of.
Our immune system uses a very low, controlled level of inflammation to manage this daily maintenance. It’s a constant, quiet process of surveillance, rectification and balancing that is essential in keeping our body in a state of healthy equilibrium called homeostasis.
The two faces of inflammation: Acute vs Chronic

To truly understand inflammation, we need to appreciate its dual nature and circumstances. Think of it like fire. A controlled fire can cook your food and keep you warm, providing comfort and sustenance. But an uncontrolled wildfire can be devastating, leaving a trail of destruction. Similarly, inflammation can be a powerful force for healing or a persistent source of damage. So, inflammation as a friend or a foe depends on whether it’s the short-lived, targeted response of acute inflammation or the slow, -simmering burn of chronic inflammation.
Acute inflammation: The body’s helpful first responder
Imagine you get a small paper cut on your finger. Within seconds, your body’s emergency response team—the immune system, springs into action. You’ll notice that the area becomes red, slightly swollen, warm, and maybe even painful. This is acute inflammation at work, and the signs of a beautifully orchestrated process. Blood vessels in the area widen to allow a rush of specialized white blood cells and healing proteins to arrive at the scene.
These first responders fight off any invading bacteria, clean up damaged cells, and lay the groundwork for repair. Once the threat is neutralized and the initial healing is done, the inflammatory response receives a clear signal to stand down. The swelling subsides, the pain fades, and your finger returns to normal. It’s a swift, efficient, and ultimately, a healing process.
Chronic inflammation: The silent, smoldering fire
Chronic inflammation is different. It’s a low-grade, systemic fire that never gets the signal to turn off. It’s not a dramatic response to an immediate injury like a cut, but a constant, dull reaction to persistent triggers such as a diet high in processed foods, ongoing psychological stress, environmental toxins, or lack of quality sleep. This is the “whispering” inflammation that doesn’t scream for attention with sharp pain or obvious swelling. Instead, it quietly and persistently damages the body over months and even years, contributing to the very feelings of being ‘off’ we talked about earlier—the fatigue, the brain fog, and the general achiness that you just can’t seem to shake. This is the inflammation that has become a key concern in modern health because of its deep connections to a host of chronic diseases.

Decoding the Whispers: 7 Common Signs of Chronic Inflammation
Chronic inflammation doesn’t announce itself with the dramatic flair of an acute injury. It speaks in subtle whispers, sending signals that are often easy to dismiss as just a part of life or stress. However, recognizing these persistent whispers is the first step towards putting off those unwanted internal fires. Here are seven of the most common signs that you might be dealing with chronic inflammation:

- Persistent fatigue and low energy: We are not talking about feeling tired after a long day. It’s a profound, lasting exhaustion that sleep doesn’t seem to fix. Your body is expending constant energy to manage the low-grade inflammatory state, leaving you feeling drained and depleted.
- Nagging body aches and joint pain: Do you wake up feeling stiff? Do your joints ache without any specific injury? Inflammatory molecules can irritate nerve endings and attack joint tissues, leading to a generalized feeling of achiness and pain, commonly in the back, shoulders, and hips.

- Brain fog and difficulty concentrating: If you find yourself struggling to focus, remember things, or think clearly, inflammation could be a key culprit. Pro-inflammatory molecules called cytokines can cross the blood-brain barrier, interfering with neurotransmitter function and contributing to that frustrating feeling of mental cloudiness.
- Stubborn weight gain (especially around the belly): Inflammation and weight often feed off each other. Belly fat—especially the deeper visceral fat(the fat stored deep in your abdomen around organs like the liver and intestines) actively releases inflammatory chemicals called cytokines. These cytokines can interfere with hormones that control hunger and metabolism, leading to increased appetite, insulin resistance, and a harder time shedding weight.

- Skin Problems: Your skin is often a mirror of your internal health. Chronic inflammation can manifest as persistent skin issues like eczema, psoriasis, acne, and premature wrinkling. By disrupting the skin’s natural barrier and repair processes, inflammation makes the skin more vulnerable to irritation, environmental stressors like UV rays and pollution.
- Digestive issues: Your gut is a major hub for your immune system. An imbalance in gut bacteria or a diet high in inflammatory foods can damage the gut lining. This can lead to a condition known as “leaky gut,” which allows particles to enter the bloodstream and trigger a systemic inflammatory response, manifesting as bloating, gas, constipation, or diarrhea.
- Frequent Colds and Infections: If you seem to catch every bug that goes around, it might be a sign that your immune system is overworked and dysregulated. Chronic inflammation keeps the immune system preoccupied, making it less efficient at fighting off actual pathogens and leaving you more susceptible to infections.
And this too is Chronic inflammation
Beyond the more recognized signs, inflammation can be the hidden root of other issues you might never connect to it.

- Mood swings and depression: The brain-inflammation connection is a rapidly growing area of research. Studies, like those published in journals such as JAMA Psychiatry, have shown a clear link between high levels of inflammatory markers (like C-reactive protein) and an increased risk of depression. Inflammation can alter brain chemistry, affecting mood-regulating neurotransmitters like serotonin and dopamine.
- Insulin Resistance: You might associate insulin strictly with diet, but inflammation plays a significant role too. Chronic inflammation can interfere with the way your cells respond to insulin, the hormone that manages blood sugar. According to the American Diabetes Association, this inflammatory-driven insulin resistance is a primary driver of prediabetes and Type 2 diabetes.
- Gum Disease (Gingivitis): That puffiness or bleeding in your gums are a sign of inflammation too. More importantly, research has shown that the inflammation in your mouth doesn’t stay there. The bacteria and inflammatory byproducts can enter the bloodstream, contributing to systemic inflammation and increasing the risk for other conditions, including heart disease.
Inflammation, immunity and age
Age is a significant, non-negotiable factor in how our bodies manage inflammation. The chronic, low-grade inflammation that often characterizes aging has its own scientific term: “inflammaging.”
A young, resilient body is highly efficient at turning the inflammatory response on and off. When a young person encounters an infection or injury, the immune system mounts a powerful, swift acute response and then quickly resolves it, returning the body to a state of balance (homeostasis). The cleanup crew is effective, and the “stand down” signals are clear and obeyed.
However, as we age, this regulatory precision begins to decline. Several factors contribute to this:
- A lifetime of triggers: Over the decades, our bodies accumulate damage from a lifetime of exposure to pathogens, environmental toxins, and cellular stress.
- Cellular Senescence: As we get older, more of our cells enter a state called senescence. These “zombie cells” stop dividing but don’t die. Instead, they remain in the body, actively secreting a cocktail of inflammatory substances that fuel the fire of inflammaging. A study published in Nature highlights that the accumulation of these senescent cells is a key driver of age-related diseases.
- Immune System dysregulation: The immune system itself ages. It becomes less effective at fighting off new invaders while simultaneously producing a higher baseline level of inflammatory cytokines.
The result is that a not-so-young body struggles to fully extinguish the flames of inflammation. The immune response becomes less targeted and more sustained, simmering constantly in the background. This persistent state of inflammaging doesn’t just make you feel older; it is now understood to be a major underlying risk factor for nearly every major chronic disease of aging, from heart disease and Alzheimer’s to arthritis and cancer. Understanding this age-related shift is crucial—it underscores why proactive anti-inflammatory habits become even more vital as the years go by.
The science of the spark: How the inflammatory process works
If you wish to truly appreciate how to cool down inflammation, you must understand the intricate genius of how the fire starts. It’s a highly organized, chain-reaction process that begins with a single, microscopic “spark”.
It all starts at the cellular level – The membranes
Your body is a country of trillions of ‘cell’ citizens. In a healthy country, each cell is in a peaceful state of balance (homeostasis), dutifully performing its job. Every cell is surrounded by an intelligent, flexible wall called the cell membrane. These cells, with their cell membranes live in a community called tissue. Apart from giving a form and holding the cell’s contents, the cell membranes monitor for physical damage, chemical irritants or unwelcomed microbes.
These cell membranes are primarily built from the fats (read fatty acids) we consume from our diet. The quality of these fats literally determines the build-quality of the walls of our country, the body – a fact that becomes incredibly important later.
While inflammation can be triggered in many ways, cell membranes are often the frontiers. When their sensors trip, they initiate a cascade of signals that sets off inflammation.
Sounding the alarm and opening the gates – the blood vessels

Once the signals are set off, they act like an emergency flare that can permeate through walls as they propel towards the nearest blood vessel. Blood vessels are like an intricate network of water pipelines in your country, the body. Two things happen as these signals reach the nearest blood vessel.
- The pipeline widens: The signals cause the blood vessels to relax, widening the vessels through a process called vasodilation. This immediately increases the volume of blood flowing to the area where the signals set off. The goal is to rush as many resources and emergency crews travelling within the blood to the scene of trouble. This surge in blood flow is precisely why an inflamed area feels warm and looks red.
- The pipe becomes leaky: Through their permeability (ability to pass through) the signals create a temporary point of entry into the blood vessel. This allows for the specialised immune cells in the blood to flow out of the blood vessel and into the affected area, typically the tissues. This intentional leakiness is also what allows fluid to seep into the area, causing the characteristic swelling.
The area is now prepped and ready for the next phase of the response.
The first responders arrive – the immune cells
The widened, leaky pipelines have successfully created an exit ramp for the emergency crews. Now, the first wave of cellular soldiers, called neutrophils, begin to arrive at the problem area. Neutrophils are part of the immune system and one of the five types of White Blood Cells. These cells constantly patrol the bloodstream (the pipelines) just waiting for a call to action.
So how do they know exactly where to go?
- Following the Scent: The neutrophils are drawn towards the site of injury by following the chemical trail left by the signals (the prostaglandins and leukotrienes). This process, called chemotaxis ensures the closer the neutrophil gets to the source of the trouble, the stronger the chemical signal becomes, guiding them with remarkable precision to the exact cells that are damaged or under attack.
- Containing the Threat: Once they arrive, these neutrophils have one primary mission: clean up and containment. Through a process called phagocytosis (which literally means “cell-eating”), they begin to engulf and digest any unwelcome microbes (like bacteria) or the debris from the body’s own damaged cells. They are working to neutralize invaders and clear away the wreckage so the healing process can begin.
The arrival and action of these neutrophils are a critical turning point. They are the first line of active, cellular defence. However, their work is intense and often messy. The battle between these soldier cells and any invading microbes is what can create pus, which is largely an accumulation of dead neutrophils, cellular debris, and fluid.
At this point, the initial alarm has been answered, and the cleanup crew is on site, working to contain the problem. But the story isn’t over; their actions will send out new signals, calling in the next wave of specialists to manage the site and begin the process of repair.
The Heavy-Duty cleanup crew arrives – The Macrophages
The initial, frantic yet crucial work of the neutrophils is like a SWAT team storming a building—effective, but it leaves a mess. Now, the second wave of responders called macrophages arrive to take control of the scene. Macrophages are another type of white blood cell whose name literally means “big eaters”. Arriving a bit later than the neutrophils, their job is more methodical and sustained.
- A more thorough cleanup: Macrophages are larger and live much longer than neutrophils. They move through the area, methodically engulfing a wider range of debris. This includes any remaining pathogens, damaged cells, and, critically, the dead and dying neutrophils that have accumulated after their initial battle. This cleanup is essential to prevent the debris from causing further irritation and prolonging the inflammation.
- The pivot to repair: This is the most crucial role of the macrophage. They don’t just clean up the past; they manage the future. As they work, macrophages release a different set of chemical signals. These new signals essentially tell the body, “The threat is contained. The cleanup is underway. It’s time to stop the battle and start rebuilding.” These signals actively suppress the pro-inflammatory response and activate the specialized cells responsible for tissue repair, such as fibroblasts, which begin to lay down new collagen to mend the damaged tissue.
The arrival and function of macrophages mark the vital pivot point in the inflammatory process. They are the key players that guide the response away from demolition and towards reconstruction, ensuring that inflammation is a temporary process that ultimately leads to healing and a return to balance. This successful transition from a pro-inflammatory state to an anti-inflammatory, pro-repair state is the hallmark of a healthy acute inflammatory response.
What’s fueling the fire? The modern causes of chronic inflammation
The beautifully orchestrated process we just described—the alarm, the cellular responders, the pivot to repair—is designed to be a short-term, life-saving event. The danger in our modern world is that this system is rarely allowed to complete its mission and stand down. Instead, it’s being constantly provoked by a host of lifestyle factors that act like a steady drip of fuel on a fire, transforming the helpful acute response into a destructive, chronic blaze. Let’s look at the main culprits.
The standard modern diet: Omega-6 vs. Omega-3
The food we eat is one of the most powerful regulators of the inflammatory dial. Central to this story are two types of essential polyunsaturated fats: omega-6s and omega-3s. We need both, but they have opposing roles. Think of omega-6s as the inflammation “accelerator” and omega-3s as the “brakes.”
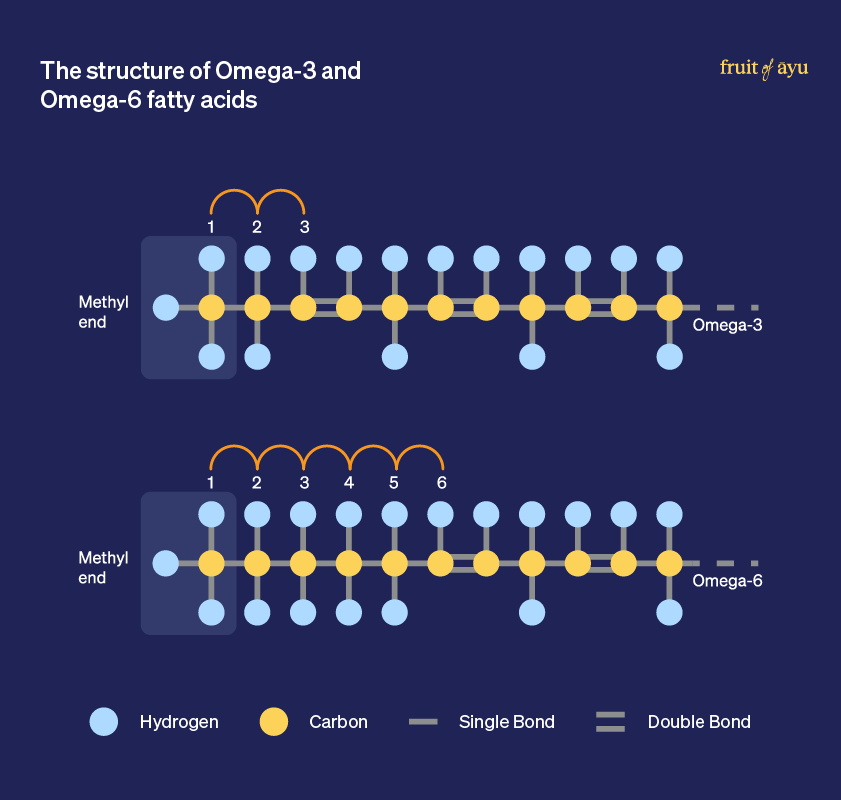
- Omega-6 fatty acids are used by the body to produce molecules that get the inflammatory process started. They are the gas pedal.
- Omega-3 fatty acids are used to create molecules called resolvins and protectins that actively resolve inflammation, telling the immune cells to stand down and initiating repair. They are the braking system.
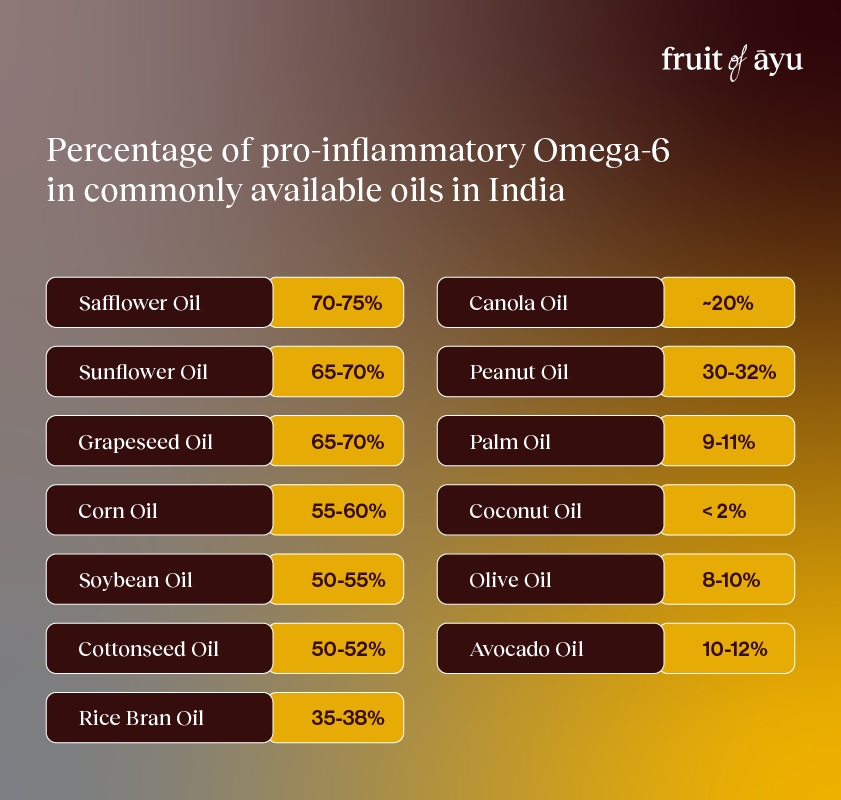
The problem is not that omega-6s are inherently bad, but that our modern diet has a dangerously skewed ratio. For much of human history, we ate these fats in a balanced ratio of around 1:1. Today, industrial seed oils (like soybean, corn, sunflower, and safflower oil) are used in nearly all processed foods. Add to that, a lower intake of omega-3 rich foods, the average modern Indian diet has a ratio as high as 45:1. This means we are constantly flooring the accelerator with very little ability to ever press the brakes, leaving the body stuck in a pro-inflammatory state.
Stress and cortisol: The mental-physical connection
Stress isn’t just in your head; it triggers a potent physical response. When you face a threat, your adrenal glands release a powerful hormone called cortisol. In the short term, cortisol is actually anti-inflammatory. It’s part of the “fight-or-flight” response that helps you survive an immediate danger.
However, when stress becomes chronic—due to demanding jobs, financial worries, or constant digital stimulation—your body is flooded with cortisol day after day. Over time, your immune cells become “resistant” to cortisol’s signal, much like cells can become resistant to insulin. This cortisol resistance means your body loses its primary tool for turning off the inflammatory response. The result is unchecked, low-grade inflammation that simmers away, driven by the very system that was meant to control it.
Lack of sleep: When your body can’t repair
Sleep is your body’s essential maintenance period. During deep sleep, your brain and body perform critical cleanup and repair tasks, including regulating the immune system. When you consistently fail to get 7-9 hours of quality sleep, you rob your body of this vital restoration window.
Sleep deprivation is a direct physiological stressor that triggers an increase in the production of pro-inflammatory cytokines. Just one night of poor sleep has been shown in studies to activate inflammatory pathways( a unique chain reaction of chemical signals that trigger inflammation) . Over time, this chronic lack of repair and increased overnight inflammation contributes significantly to the overall systemic fire, leaving you feeling groggy, achy, and mentally foggy.
A sedentary lifestyle: Movement as an anti-inflammatory
Our bodies were designed for movement. A sedentary lifestyle, common in today’s office-based world, promotes inflammation. Fat tissue, particularly visceral fat around the organs, like we discussed before, secretes low-grade inflammatory signals.
Conversely, regular physical activity is one of the most effective anti-inflammatory tools we have. During and after exercise, your muscles release compounds, including a myokine called IL-6, that has a systemic anti-inflammatory effect. Moderate exercise helps reduce visceral fat, improves insulin sensitivity, and enhances your body’s antioxidant defenses. When you don’t move enough, you miss out on this powerful, free, and natural anti-inflammatory medicine.
Environmental toxins and gut health
We are constantly exposed to a low level of toxins in our environment, from air pollution and plastics to pesticides and heavy metals. This places a constant burden on our body’s detoxification and immune systems, contributing to chronic inflammation.
Nowhere is this more critical than in our gut. Your gut is a major barrier between the outside world and your internal system, and it houses the majority of your immune cells. A poor diet, stress, and toxins can disrupt the delicate balance of your gut microbiome, leading to a condition known as “leaky gut” (increased intestinal permeability). This allows partially digested food particles and bacterial toxins to “leak” into the bloodstream, where they are seen as foreign invaders. Your immune system rightfully launches an attack, creating a state of continuous, systemic inflammation that originates from your digestive tract.
Your anti-inflammatory action plan: How to put out the fire
Understanding the science and the causes of chronic inflammation is the first step towards change, but knowledge becomes power only when it’s put into action. The good news is that you have significant control over the factors that fuel this fire. By making conscious, consistent choices, you can turn down the heat, rebalance your body, and reclaim your health. This isn’t about perfection; it’s about progress. Here is your practical action plan.
Eat an Anti-Inflammatory Diet
You cannot build a healthy, fire-resistant house with flammable materials. The single most impactful change you can make is to shift your diet from one that promotes inflammation to one that actively fights it. This doesn’t mean giving up Indian food; it means embracing the traditional, wholesome ingredients that have always been at its heart.
Foods to embrace
- Oily Fish: Mackerel (Bangda), Sardines (Mathi/Tarlī), and Hilsa (Ilish) are excellent sources of the powerful anti-inflammatory omega-3 fatty acids. Aim for at least two servings per week if you are non-vegetarian.
- Local leafy greens: Spinach (Palak), Fenugreek leaves (Methi), Amaranth leaves (Chaulai/Thotakura), and Drumstick leaves (Munagaku) are nutrient powerhouses, rich in antioxidants that protect your cells.
- Deeply colored Fruits: Pomegranate (Anaar), Jamun (Indian Blackberry), and Amla (Indian Gooseberry) are loaded with protective compounds and Vitamin C, which have potent anti-inflammatory effects.
- Nuts and seeds: Walnuts (Akhrot), Almonds (Badam), Flaxseeds (Alsi), and Sesame seeds (Til) provide a mix of healthy fats, fiber, and antioxidants.
- Healthy fats & oils: Prioritize traditional fats like Ghee (used in moderation) and cold-pressed (kacchi ghani) Mustard Oil and Groundnut Oil over highly refined vegetable oils that are high in Omega-6s.
- Essential Spices: The soul of Indian cooking is already anti-inflammatory! Turmeric (Haldi), Ginger (Adrak), Garlic (Lehsun), Cinnamon (Dalchini), and Cloves (Laung) are all powerful, well-researched inflammation fighters. Use them generously.
Foods to limit
- Packaged & processed snacks: This includes biscuits, chips, instant noodles, and other packaged foods that are typically made with refined flour (maida), unhealthy fats, and preservatives.
- Sugary drinks and sweets: Greatly reduce intake of packaged fruit juices, sugary sodas, sherbets, and excessive consumption of mithai. These cause sharp spikes in blood sugar, a major driver of inflammation.
- Refined carbs & flours: Limit foods made from maida, such as naan, white bread, and many baked goods. Be mindful of a diet overly reliant on polished white rice. Opt for whole grains like atta, ragi, and jowar.
- Deep-fried foods: Minimize deep-fried items like samosas, pakoras, and puris, especially those from commercial establishments where oil is often reused, creating highly inflammatory compounds.
- Unhealthy fats: Avoid or eliminate refined vegetable oils (often sold as generic “vegetable oil” or “sunflower oil”) and hydrogenated fats like Vanaspati (Dalda), which contain harmful trans fats.
Master your stress
You can’t eliminate stress from your life, but you can change your response to it to protect your body from its inflammatory consequences. To achieve this, activate your body’s relaxation response.
- Practice Mindfulness: Just 5-10 minutes of daily mindfulness meditation can lower stress hormones.
- Breathe Deeply: When you feel stressed, practice “box breathing”: Inhale for a count of 4, hold for 4, exhale for 4, and hold for 4. Repeat several times to calm your nervous system.
- Get Outside: Spending time in nature, also known as “forest bathing,” has been shown to lower cortisol, blood pressure, and inflammation.
- Seek support from family and friends: In times of stress, withdrawing is a common instinct, but reaching out is a powerful remedy. Talk to your family, friends, or a trusted confidant about what you’re feeling. Sharing your burdens can lighten the load, provide a fresh perspective, and strengthen the social bonds that are fundamental to our emotional well-being and resilience. A simple conversation can be one of the most effective forms of stress relief.
Prioritise quality sleep (7-9 hours)
Sleep is non-negotiable for immune health. Treat it with the same importance as diet and exercise. Create an environment that promotes deep, restorative rest.
- Stick to a schedule: Go to bed and wake up around the same time each day, even on weekends, to regulate your body’s internal clock (circadian rhythm).
- Create a sanctuary: Keep your bedroom dark, cool, and quiet. Use blackout curtains, an eye mask, or a white noise machine if needed.
- Have a digital sunset: Avoid screens (phones, tablets, TVs) for at least an hour before bed. The blue light they emit can suppress melatonin, the hormone that signals your brain it’s time to sleep.
Move your body intelligently
The goal is consistent, balanced movement—not necessarily punishing, high-intensity workouts every day.
- Aim for Consistency: A brisk 30-minute walk most days of the week is more beneficial than one intense gym session on the weekend.
- Build Muscle: Strength training (using weights, bands, or your bodyweight) builds metabolically active muscle, which helps regulate blood sugar and reduces inflammation.
- Don’t Forget to Stretch: Incorporate gentle movement like yoga or simple stretching. This not only improves flexibility but also helps lower stress hormones and calm the nervous system.
From feeling ‘Off’ to taking control
We started this journey by trying to put a name to that vague, nagging feeling of being ‘off’. We now have pointers that determine if these are the whispers of chronic inflammation. You’ve learned that inflammation isn’t inherently bad and that it is a vital, healing force under controlled circumstances. The problem is the uncontrolled, smouldering fire of chronic inflammation, quietly fueled by the triggers of our modern lives.
But the goal of this journey was not to leave you with a sense of alarm, but with a sense of agency. Understanding the science, the signs, and the causes is empowering because it illuminates the path forward. The most important takeaway is that you have significant control over this process.
The action plan outlined above is not an all-or-nothing prescription. It’s a toolkit. Don’t feel overwhelmed by the need to change everything at once. Lasting change is built on small yet consistent steps.
Perhaps this week, you focus on adding a portion of leafy greens to your daily meals. Maybe you decide to take a 20-minute walk after dinner each night. Or perhaps you commit to putting your phone away an hour or thirty minutes before you sleep. Each of these small victories is a step towards quenching the fire. Each conscious choice sends a powerful message to your body that you are shifting the balance from a state of stress to a state of healing.
You are not destined to simply feel “off.” By understanding the whispers of your body and making mindful choices, you can put out the fire and take back control of your well-being, one small step at a time.